Please view the December 2021 Case of the Month below:
Clinical Cases from Emory Division of Hospital Medicine Annual Clinical Vignette Conference
“A Flying Crisis”
Submitted by:
Willie Smith, MD
Assistant Professor & Master Clinician
Division of Hospital Medicine
Emory Department of Medicine
Vana Bollineni, MD
Assistant Professor
Division of Hospital Medicine
Emory Department of Medicine
Jennifer Xu, MD
Assistant Professor
Division of Hospital Medicine
Emory Department of Medicine
Edited by Yelena Burklin, MD, FHM, FACP
CASE
A 19-year-old male with a history of asthma, sickle cell trait, and right lower extremity benign osteochondroma post-resection, presented with a sharp left upper quadrant abdominal pain that has developed suddenly, following prolonged air travel. He denied other associated gastrointestinal symptoms, fevers, trauma, or alcohol use. His vital signs upon admission to the hospital were within normal limits, and physical examination revealed the presence of a tender palpable edge of the spleen in the left upper quadrant of the abdomen.
Laboratory findings were notable for an elevated total bilirubin level at 3.4 mg/dL and a white blood cell count of 10.6 x 103 /µl. Viral serologic testing for HIV, hepatitis A/B/C panel, EBV, and CMV, were all negative. The PCR testing for COVID-19 was also negative. Hemoglobin electrophoresis was obtained and revealed Hemoglobin S of 37.6%, confirming the presence of a sickle cell trait.
Additional testing, including hypercoagulable panel and antiphospholipid antibody presence, was negative, as well.
Transthoracic echocardiogram was unremarkable, with no evidence of valvular abnormalities, intramural thrombi, or masses.
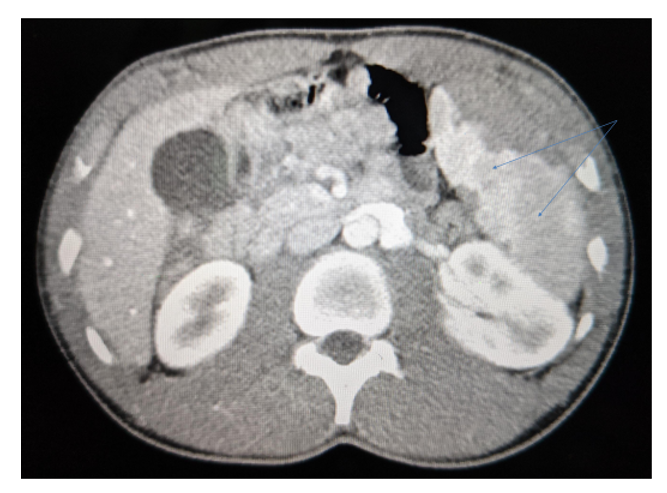
The image of his computed tomography of abdomen and pelvis is provided below:
What is your diagnosis?
Computed tomography (CT) of the abdomen and pelvis was notable for the presence of mild splenomegaly and evolving splenic infarcts without evidence of splenic artery thrombosis.
FINAL DIAGNOSIS
High-altitude related splenic infarct in a person with a sickle cell trait.
Hospitalization course:
Patient was conservatively managed with analgesic regimen (NSAIDs and opioids for severe pain) and discharged to follow-up in the hematology clinic.
DISCUSSION
Sickle cell trait (SCT) is one of the rare causes of splenic infarction. Few high altitude-related splenic infarcts in the SCT population were reported in the literature.
It is hypothesized that the hypoxemic stress induced by a high altitude, in combination with the increased percentage of Hemoglobin S (HbS) present in the blood – are two predisposing factors for the development of splenic infarction. In uncomplicated cases of splenic infarction, the condition is managed with a conservative regimen only. Symptoms spontaneously resolve between 7 and 14 days. Splenic rupture and the need for splenectomy in these cases are extremely rare. However, in cases of complicated splenic infarcts that result in splenic rupture, abscess, sequestration crisis, or chronic pain despite supportive therapy – surgical splenectomy should be considered.
Even though splenic infarction associated with SCT is rare, it needs to be considered in patients who present with sudden abdominal pain after being exposed to high altitudes. Once splenic infarction is diagnosed, hemoglobin electrophoresis needs to be included as part of the diagnostic process. The majority of cases are treated conservatively, however, early identification and proper management of splenic infarction in this setting help avoid life-threatening complications that may require complex surgical interventions.
CITATIONS
- O’Brien RT, et al. Splenic Infarct and Sickle-(Cell) Trait. N Engl J Med, 1972. 287(14): p. 720-720
- Nair, V, et al. Splenic Infarct as A Harbinger for Sickle cell Traits in High Altitude. Blood, 2017. 130(Supplement 1): p. 4650-4650


Be the first to comment on "Faculty Development Case of the Month: December 2021"